THE probiotici intestinali, noti anche come fermenti lattici, rappresentano un’eterogenea popolazione di specie batteriche residente nel nostro apparato digerente. Essi sono indispensabili per la vita dell’uomo grazie ad alcune funzioni svolte, come sintesi di vitamine e modulazione del sistema immunitario. Main characteristics, functions and properties of probiotics will be collected in this article.
Intestinal Probiotics - Introduction
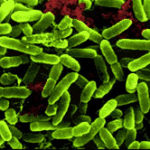
Bacteria, which normally also reside in our intestines, were the first inhabitants of the earth, when there was still no oxygen in the atmosphere, subsequently they adapted to the optimal environment of the interior of the intestine of the most evolved organisms in which they found hot, humid, lack of oxygen, darkness and food.
The bacterial population residing in our digestive tract is made up of more than 100,000 billion units, a figure equal to at least 10 times the total number of cells that make up an adult man, for a total weight of about 1.5 kg.
Considering such a large number of units, the entire intestinal bacterial population can be understood as a real organ, or rather a meta organ, able to exert an important influence on the daily and physiological activities of man. Within this vast microbial population, about 500 different bacterial species coexist. Germ free laboratory animals, ie animals artificially deprived of intestinal bacteria from birth, grown in a glass hood, are small and thin.
Colonizzazione dell’intestino da parte dei batteri – i probiotici intestinali
The composition of the bacterial flora varies considerably from the mouth to the colon: the particular physiology of the various segments of the digestive system, bathed by different secretions and characterized by different movements, favors the development of heterogeneous microbial populations.
Numerosi sono i fattori che influenzano la composizione dei probiotici intestinali alla nascita: il tipo di parto, l’alimentazione, la qualità dei servizi ospedalieri ed i trattamenti con farmaci antibiotici. Il canale digerente dell’uomo risulta sterile fino al concepimento, poi, già dai primi momenti di vita, durante il passaggio attraverso il canale del parto, viene colonizzato da un’enorme varietà di specie microbiche. Nei bambini nati con parto cesareo la colonizzazione del tratto gastrointestinale avviene invece tardivamente, intorno alla terza-quarta giornata di vita, ad opera dei microrganismi presenti nell’ambiente ospedaliero, per cui la loro microflora differirà da quella materna.
At birth, when the space and nutrients available to microorganisms are abundant, in the gastrointestinal tract the bacteria that have a high speed of reproduction dominate; with the passage of time, however, the number of microorganisms grows and the nourishment and space available begin to run out, so only the most highly specialized microbial species survive.
Regarding the type of feeding, in breastfed babies, the intestinal microflora is almost entirely made up of Bifidobacteria is Lactobacilli, but after weaning the appearance changes: i Clostridia and numerous are formed Bacteroids, the Eubacteria and of Peptococci. This is how the innumerable bacterial types that lodge in the gastrointestinal tract of an adult individual begin to be defined.
Although consolidated already after the first years of life, the bacterial population (the microbiota) may later be modulated by lifestyle, stress, smoking, physical activity, drugs, ingested food and other factors, some of which are yet to be defined.
Some bacterial strains are common to the majority of humanity; 80% of bacteria causes the fermentation(decomposition of carbohydrates for energy), such as Lactobacillus is Bifidobacteria, and the remaining 20% causes the rot (decomposition of proteins by anaerobic bacteria), such as Escherichia, Bacteroides,Eubacteria, Clostridium.
Many of these bacteria are useful or harmless as constituents of the microbiota, while others could become pathogenic if allowed to proliferate without the control of the immune system and other bacterial populations.
Among the components of the human microbiota, some of the most representative species, generally harmless and useful for humans, are listed below:
Acinetobacter calcoaceticus, Alcaligenes faecalis, Anaerobiospirillum, Bifidobacteria breve, Bifidobacteria infantis,Bifidobacterium lactis, Bifidobacteria longum, Enterococcus fecalis, Lactobacillus acidophilus, Lactobacillus casei,Lactobacillus delbrueckii, Lactobacillus plantarum, Lactobacillus rhamnosus, Staphylococcus faecium, Streptococcus salivarius thermophilus.
On the other hand, some bacterial species can become dangerous for the life of the host if they invade other organs or replicate in an uncontrolled manner. Their proliferative activity is controlled by the immune system and by competition with other intestinal microorganisms for nourishment and space. Among the main ones are listed the following species:
Bacteroides fragilis, Candida albicans, Clostridium, Enterococcus faecium, Eubacterium nodatum, Escherichia coli Nissle,Fusobacterium, Peptococcus, Peptostreptococcus, Plesiomonas shigelloides, Porphyromonas gingivalis, Ruminococcus.
Function of the microbiota
I microbi non sono dei semplici commensali, ma hanno delle precise funzioni metaboliche e immunologiche. Essi sono fondamentali per la nostra salute: molti studi confermano, ad esempio, che le persone obese hanno una composizione dei probiotici intestinali diversa dalle persone magre, se sia la composizione alterata del microbiota la causa dell’obesità o la sua conseguenza è ancora oggetto di studio, ma in ogni caso si è visto che trapiantare il microbiota di un animale grasso in uno magro fa sì che quest’ultimo diventi grasso e viceversa, tutto questo significa che probabilmente esso controlla anche l’aumento di peso dell’uomo. Inoltre, modificando il microbiota di un diabetico, si possono controllare la glicemia e l’insulino-resistenza.
Più in generale il microbiota invia tutta una serie di segnali in un sistema che lo collega al tessuto adiposo, al pancreas, al fegato, al cervello, organi che sono continuamente in contatto tra loro. Tutto questo si traduce nella possibilità di comunicare al cervello ciò che si deve mangiare e ciò che si deve assorbire e forse finisce con l’influenzare anche il nostro modo di pensare ed il nostro comportamento.
The development of the microbiota goes hand in hand with the GALT (Gut Associated Lymphoid Tissue), i.e. the intestinal immunological system, which will be educated by it and that microbiota will then be tolerated by that immune system. This is not a negligible aspect if you think that the 70% of the cells that make up the human immune system is located in the intestine.
This biosystem, with which our body is confronted every day, is not static, but is characterized by a dynamic balance between the different bacterial species, maintaining a fairly constant composition in the same individual even in the presence of variable environmental and dietary conditions.
The alteration of homeostasis, i.e. the balance of bacterial species of the microbiota, is known as dysbiosis and can lead to more or less serious consequences such as colonization by the Clostridium difficile (a species of bacteria extremely resistant to antibiotics that causes diarrhea and intestinal malabsorption); dysbiosis can also be the cause of disorders and diseases that affect the digestive system such as dyspepsia (digestive disorders), irritable bowel syndrome and chronic intestinal diseases.
Any change in the balance of the intestinal bacterial population significantly affects the course of many diseases, including obesity, the allergic states, the inflammatory bowel diseases and metabolic pathologies.
La mappatura dei probiotici intestinali può essere richiesta dai medici di base o dai centri clinici di riferimento per le patologie associate alle alterazioni della flora batterica intestinale. Il test disegna una mappa genetica completa delle specie di batteri che compongono il microbiota individuale, insieme a una mappa biochimica, ovvero un quadro complessivo di come questi batteri interagiscono tra di loro e come si modificano in rapporto allo stato di salute o di malattia. Tali informazioni si rendono utili ai fini diagnostici per eseguire interventi mirati a riequilibrare la popolazione dei microbi intestinali attraverso l’ottimizzazione della dieta, la somministrazione di probiotici, fino al trapianto di microbiota.
Balance of intestinal bacteria and main strains
Il microbiota è un biosistema aperto; esso è popolato da specie batteriche residenti, chiamate autoctone, e da una variegata popolazione di specie transitorie, definite alloctone, che comprendono sia microrganismi il cui habitat naturale è localizzato altrove nel tubo digerente sia le notevoli quantità di batteri che vengono ingeriti con gli alimenti. Il microbiota intrattiene rapporti continui con il mondo esterno ed è sottoposto ad incessanti movimenti, sia in entrata sia in uscita (espulsione di batteri attraverso le feci). Nonostante ciò, la composizione dei probiotici intestinali tende a mantenersi costante nel tempo. I principali fattori che permettono il raggiungimento e il mantenimento di questo equilibrio, pur con ampie variazioni individuali sono:
- Gastric secretion: the acid juice produced by the stomach is a powerful bactericide, capable of controlling the reproduction of microorganisms present in food and saliva. THE proton pump inhibitor drugs and antacid drugs can in fact cause dysbiosis since, by altering the gastric pH, facilitating the passage of pathogenic bacterial strains in the intestine, which, in conditions of physiological gastric acidity, would not survive.
- Oxygen contained in the intestine: regulates the distribution and activity of aerobic microorganisms that need oxygen to live, removing it from the environment, facilitating the growth of anaerobic strains.
- Peristaltic activity: helps to keep the composition of the bacterial flora constant, continuously exposing the gastrointestinal tract to a great variety of bacteria from the external environment, to food (whose mixing promotes a continuous elimination of microorganisms) and to gastric, pancreatic and biliary secretions.
- Interactions between microorganisms: l’equilibrio della flora batterica dipende molto anche dai rapporti fra le differenti specie di probiotici intestinali che la popolano e che hanno trovato, nel tempo, le condizioni per convivere in modo equilibrato, condividendo gli spazi, il cibo e aiutandosi reciprocamente, come per esempio nel caso di batteri aerobi ed anaerobi, o impedendo ai microrganismi patogeni di colonizzare il loro territorio.
Food supplement
Un modo per garantire, modulare ed influenzare positivamente l’equilibrio della flora batterica intestinale è quello di introdurre in questo ecosistema microrganismi vivi, appartenenti a specie considerate benefiche per la salute: questi organismi vengono chiamati probiotici intestinali dal greco pro + bios, or "for life", "for life". A food can therefore be defined as a probiotic when, thanks to the presence, in high quantities, of live probiotic microorganisms, it is able to modify the balance of the intestinal bacterial flora and strengthen the immune defenses, thus contributing to the improvement of health.
Among the microorganisms used in probiotic foods, i lactic bacteria; these are gram-positive non-pathogenic microorganisms that are capable of producing lactic acid as an end product of the primary metabolism.
Lactic acid bacteria include several bacterial species such as i Lactobacilli, i Lactococci he Streptococci. THE Lactobacilli they have extremely variable characteristics: they may in fact have a different genetic makeup and different ability to adhere to the intestinal epithelium and colonize it; therefore any particular type of Lactobacillus it must be studied individually to identify its probiotic properties and beneficial effects on human health.
Affinché un alimento o integratore di probiotici intestinali possa essere utilizzato nella prevenzione e nel trattamento di malattie o disordini a livello del tratto gastrointestinale, deve essere sicuro e per questo appartenente alla popolazione di microrganismi che normalmente vivono nell’intestino. Inoltre, un fattore estremamente importante da considerare per determinare l’efficacia di un microrganismo probiotico è la sua abilità di sopravvivere all’ambiente acido e all’azione proteolitica degli enzimi digestivi del tratto gastrointestinale; molti microrganismi infatti non resistono al pH acido dello stomaco o alle secrezioni biliari del duodeno.
Caratteristiche richieste ai probiotici intestinali assunti con la dieta o l’integrazione alimentare:
- General requirements: no risk for immunosuppressed subjects, intestinal origin, resistance to both the acidic and neutral environment and to the proteolytic action of digestive enzymes and to the bile produced by the liver;
- Technological requirements: ability to survive in the period of marketing (shelf-life), not to be responsible for the production of acid compounds;
- Functional requirements: inhibition action on pathogenic bacteria, ability to adhere to the intestinal epithelium with a barrier function, intestinal colonization, inhibition of pro-carcinogenic enzymatic activity in the intestine.
As for the use of prebiotici intestinali, these are substances that cannot be digested by the human digestive system, capable of selectively stimulating the proliferation and activity of one or more beneficial bacteria, providing them with nourishment; particularly useful is theinulin from chicory or from agave.
Invecchiamento e probiotici intestinali
La longevità è un tratto complesso in cui giocano un ruolo chiave la genetica, l’ambiente e il caso. Influenzando molteplici aspetti della fisiologia umana, come il corretto funzionamento del sistema immunitario e del metabolismo energetico; i probiotici intestinali possono rappresentare un tassello importante nel definire come e quanto un essere umano può invecchiare mantenendosi in buona salute.
Recenti studi hanno tuttavia dimostrato che l’abbondanza cumulativa delle specie batteriche costituenti i probiotici intestinali diminuisce con l’avanzare dell’età, favorendo la progressiva proliferazione di specie definite sub dominanti e opportunisti ad azione pro infiammatoria, presenti in ridotte concentrazioni nell’intestino dei giovani adulti.