Means vitamin D, or calciferols, a series of compounds with antirachitic action, that is necessary to prevent the rickets disease characterized by severe ossification disorders with consequent bone deformations and mental retardation.
Vitamin D2, or ergocalciferol, was the first antirachitic compound to be isolated from ergot mushroom (Claviceps purpurea), a pest of grasses.
Vitamin D3, or cholecalciferol, was subsequently isolated from fish oil. Both of these forms are inactive: bio-activation occurs as a result of the reaction between liver enzymes and vitamin D. It is important to underline that vitamin D3 will be, after bio-activation, 80-100 times more active than vitamin. D2.
Among the products obtained from the enzymatic reaction, the calcidiol (25-hydroxycholecalciferol), a prehormone, which in turn is transformed by the same liver and kidney enzymes into the final active hormone calcitriol (1,25-dihydroxycalciferol or 1,25- (OH)2D).
Calcitriol interacts with intracellular receptors located near the cell nucleus, activating them. It plays an essential role in the regulation of calcium and phosphorus metabolism:
- promotes the absorption of calcium in the intestine;
- promotes the reabsorption of calcium and phosphorus in the proximal convoluted tubule;
- favors the deposition of calcium in the bone tissue.
Furthermore, calcitriol exerts an effect on cell growth and differentiation on the skin, induces the formation of macrophages (cells of the immune system) starting from myeloid precursors, inhibits the synthesis of immunoglobulins and stimulates platelet aggregation.
Man is also able to synthesize vitamin D from provitamin dehydrocholesterol, a chemical compound similar in molecular structure to cholesterol, located on the surface of our skin. The dehydrocholesterol, irradiated by the sun, can be transformed into cholecalciferol (vitamin D3), through a chemical reaction catalyzed by ultraviolet rays (UV) and in turn transformed into 1,25-dihydroxycalciferol by the enzymes of the liver and kidney.
Thanks to the presence of dehydrocholesterol in our skin, adequate exposure to the sun reduces the need for vitamin D. However, there are several factors that reduce the absorption of sunlight by the skin, counteracting the formation of vitamin D, such as:
- increased pigmentation of melanin,
- hyperkeratosis,
- use of sun filters (e.g. sun creams),
- poor sun exposure,
- shortness of the hours of sunshine,
- obliquity of the sun's rays (winter period),
- presence of smog with consequent reduction of the penetration of UV rays.
How much vitamin D does the sun generate on our skin?
By exposing the body surface 100% to the sun for the time necessary to produce a mild erythema (about 30-45 minutes in the summer), a plasma increase in vitamin D concentration is guaranteed, equivalent to taking an oral dose of cholecalciferol equal to to 1,000 IU (equal to 25 micrograms), a concentration useful for the daily requirement of a healthy person for 3-5 days.
Sources of vitamin D.
The foods richest in vitamin D are liver, fish oils, some marine fish (herring, salmon, sardine). Smaller quantities are present in eggs, butter and milk.
Daily requirement of vitamin D
According to Regulation (EU) No. 1169/2011 of the European Parliament and of the Council of 25 October 2011, the recommended consumption of vitamin D is 5 mg of vitamin D. Under normal conditions, good exposure to the sun and a varied diet is sufficient to satisfy the body's needs for calciferol. However the doctor can prescribe integratori alimentari di vitamina D is Football, antioxidant supplements or even drugs (Dibase® or Didrogyl®) in case of vitamin deficiency or in the presence of risk factors.
Vitamin D deficiency
La carenza di vitamina D è la condizione clinica derivante dall’assenza di appropriati livelli di vitamina D nell’organismo. Secondo l’Università di Harvard, la carenza di vitamina D riguarderebbe circa un miliardo di persone nel mondo.
The main consequences of vitamin D deficiency are rickets in young subjects and osteomalacia and osteoporosis in adults.
The diagnosis of vitamin D deficiency is performed with a blood test, more in detail the quantity of calcidiol prehormone per volume of blood is sought:
| Condition | Concentration in nmol / l | Concentration in ng / ml |
| Shortage | <30 nmol / l | <12 ng / ml |
| Insufficiency | Between 30 nmol / l and 75 nmol / l | Between 12 ng / mL and 30 ng / mL |
| Normality | Between 75 nmol / L and 200 nmol / L | Between 30 ng / mL and 80 ng / mL |
| Excess | > 200 nmol / l | > 80 ng / ml |
| Toxicity | > 375 nmol / l | > 150 ng / ml |
Causes of deficiency:
Vitamin D deficiency can be caused by:
- insufficient intake with food;
- poor sun exposure;
- impaired intestinal absorption capacity;
- liver and kidney diseases that compromise the production of enzymes responsible for the bio-activation of vitamin D;
- use of drugs such as cholestyramine, glucocorticoids, antifungals, antivirals, anti-rejection drugs etc ... that compromise the normal metabolism of vitamin D.
There are also risk factors associated with a greater risk of developing vitamin D deficiency; among the main ones:
- obesity: vitamin D, being similar to fatty tissues, is sequestered by the latter, with a reduction in bioavailability;
- cigarette smoking and alcoholism: impaired enzymatic metabolism of vitamin D;
- advanced age: the skin, with increasing age, progressively loses its ability to produce vitamin D;
- Crohn's disease or celiac disease: impaired intestinal absorption of vitamin D;
- Babies who are breastfed for a long time may be deficient in vitamin D, as breast milk is a scarce source.
Deficiency symptoms and associated diseases
Vitamin D deficiency is a devious condition. However serious deficiencies can show a symptomatic picture characterized by:
- pain in bones, joints and muscles;
- recurrent fatigue;
- brittle bones that tend to deform;
- neurological disorders (difficulty thinking clearly).
Vitamin D deficiency impairs bone mineralization in different ways, which contributes to the development of diseases such as rickets in children and osteomalacia and osteoporosis in adults. However, recent studies associate vitamin D deficiency with diseases such as diabetes, hypertension, metabolic syndrome and dyslipidemia.
Deepening: Bone Diseases
There are a series of pathologies of different nature (etiology) that affect the skeletal system as a whole; they are very complex from a pathogenetic point of view.
Factors such as nutritional deficits, genetic anomalies affecting the connective tissue or cells involved in bone remodeling (osteoblasts and osteoclasts) are generally involved, or alterations in the synthesis of the hormones that regulate calcium metabolism, or calciumotropic hormones.
Among the numerous pathologies that can affect the skeletal system, the most widespread and common are those characterized by bone demineralization or a reduction in bone mass. These certainly include osteomalacia ed osteoporosis.
Symptoms
Symptoms in adult subjects suffering from osteomalacia and osteoporosis are pain, the presence of spontaneous fractures or minimal trauma and the appearance of bone deformities, while in children it generally manifests itself as a reduced increase in stature.
The first clinical manifestation of the disease is often a fracture, usually in the vertebral or neck of the femur. However, in some cases the disease remains asymptomatic for a long time and can only be revealed by specific laboratory tests. Unfortunately, bone diseases due to demineralization show a degenerative trend, so if not properly treated, they get worse over the years.
Osteomalacia
Osteomalacia is a pathology characterized by inadequate mineralization of the newly formed bone matrix that appears in the adult after the welding of the junction cartilages.
The most common cause of osteomalacia is, as already mentioned, the nutritional deficiency of vitamin D, therefore caused by an insufficient intestinal absorption of this vitamin or by its altered metabolism, or, more rarely, by a genetic deficiency that prevents the use of the vitamin itself. In turn the deficiency or functional insufficiency of vitamin D causes insufficient intestinal absorption of football and other minerals that make up the bone matrix such as phosphates is magnesium.
A further cause of osteomalacia is secondary hyperparathyroidism which produces calcium release from the bones and decreased renal calcium clearance (which corrects hypocalcemia) at least in the early stages of the disease. If left untreated, osteomalacia can develop into osteoporosis.
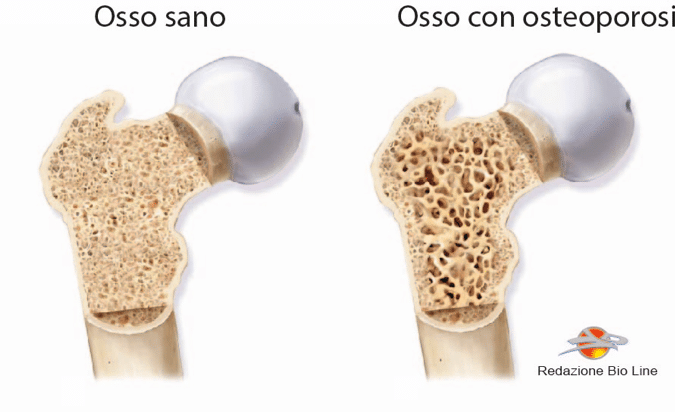
Osteoporosis
The main characteristics of osteoporotic bone are the decrease in thickness and increase in porosity of the cortical bone, and the reduction in the number and size of transverse trabeculae (the unit of organization of bone tissue). Osteoporosis is associated with an increased risk of fracture, which, as already mentioned, is the main clinical symptom of the disease.
The main risk factors associated with osteoporosis are:
- old age;
- immobilization, no load;
- endocrine abnormalities (lack of estrogen, both male and female hypogonadism, adrenal hyperactivity, primary hyperparathyroidism);
- drugs (chronic therapies with cortisone);
- diseases that cause intestinal malabsorption;
- menopause;
- intake of reduced amounts of minerals (calcium) and vitamin D;
- inheritance.
Osteoporosis can be defined as primary or secondary. The main difference between the two types is that primary osteoporosis is closely associated with aging and the cessation of ovarian activity (menopause), while the secondary arises from other diseases or the use of drugs and substances:
- Endocrine system abnormalities: hyperparathyroidism, hypogonadism;
- Bone marrow tumors;
- Chronic corticosteroid therapy;
- Cushing's syndrome;
- Liver and gastrointestinal disorders leading to malabsorption of vitamin D and calcium;
- Alcoholism, as alcohol is an inhibitor of osteoblastic activity.

