Allergy
The response of the immune system against harmless substances and drugs: an overview of the mechanisms of activation of the allergy and of the main pharmacological therapies available.
It is estimated that around 20% of the world population suffers from one or more forms of allergy. The term allergy it was coined in 1904 by the Austrian pediatrician C. von Pirquet, and it is an immune-based reaction of an organism following previous contact with substances such as microorganisms, toxins, protein bodies.
Allergy-causing substances are called allergens.
Obviously, the tissues most prone to allergic reactions are those most exposed to the external environment such as skin, respiratory tract and digestive system, in which we can generally have mild forms, while when the reaction affects the blood, a very serious form of reaction called anaphylaxis, which, if not promptly treated, can lead to death.
The immune system as the main responsible for the allergic reaction
Our body is equipped with an efficient immune system which has the function of defending itself from the harmful action of foreign or harmful substances by producing antibodies, substances able to selectively bind the pathogen to destroy it. Antibodies are protein-based immune mediators that specifically recognize a small protein part of the allergen, called antigen. The antibodies by binding to their own antigen trigger a reaction at the binding site, which activates the white blood cells of the immune system, macrophages, T lymphocytes and basophils. These cells release organic chemicals, such ashistamine and of leukotrienes responsible for the allergic reaction with more or less intense itching, runny nose, cough or breathlessness, and sometimes even for a substance apparently harmless for most people, such as flower pollen, foods such as shellfish, gluten, sulphites, or the same tissues of the body.
Role of histamine and allergy drugs
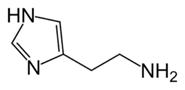
Fig. 1 - Molecular formula of histamine
Histamine (Fig. 1) is ubiquitous in the body, found in the central nervous system (CNS) and in all tissues of the body, especially those in contact with the external environment. It is synthesized from the amino acid histidine and stored in mast cells.
Histamine works by binding to its own H receptors1 placed in the tissues of the body; antihistamine drugs specifically bind to these receptors by occupying the histamine binding site without activating them.
Antihistamine drugs are used to treat localized allergy disorders such as allergic rhinitis, urticaria and contact dermatosis, when histamine is the only chemical mediator.
On the contrary, they are not useful for other manifestations such as asthma, food allergy and anaphylactic shock, because histamine is not the only mediator in these processes.
The H receptors1 are also placed in the CNS, where histamine, even in the absence of an allergic reaction, has an exciting action, so that the massive block of H receptors1 on the part of non-selective antihistamine drugs causes drowsiness.
The newer drugs are more selective for receptors located outside the CNS and therefore induce less sleepiness; however they are not without other side effects such as anticholinergic effects (dry mouth and airways, hypertension) and cardiac toxicity. Terfenadine (Teldane®) entered therapy in the 1990s but, due to its influence on the heartbeat, was withdrawn from the market.
Among the most used antihistamine drugs: cetirizine (Circle®, Formistin®, Zirtec®), fexofenadine (Telfast®), loratadine (Clarityn®), desloratadine (Aerius®, Azomyr®), ebastine (Kestine®).
Another class of drugs used against the most serious allergic reactions such as allergic asthma or anaphylactic shock, arecortisone. These drugs have an immunosuppressive action by blocking the action of immune cells. However, the main action of cortisones remains the blocking of the production of inflammatory mediators, starting from the arachidonic acid cascade.
THE NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) they should not be taken to treat allergy symptoms as they induce a greater release of leukotrienes, responsible for bronchospasm and worsening of asthma symptoms.
L'adrenaline it is used as an emergency treatment for anaphylactic shock; is a powerful vasoconstrictor which, when injected, causes blood pressure to rise and stimulates the heartbeat. The administration takes place only by injection, because it is not absorbed if taken orally. There are pre-filled syringes on the market containing a dose of adrenaline inside which is useful for a first emergency intervention in case of anaphylactic shock.
How are allergic reactions classified?
Allergic reactions, based on the activation mechanism and symptomatology, can be divided into four types:
- Type I hypersensitivity reaction (or anaphylactic): it is generated in response to widespread environmental antigens, allergens, which cause the production of specific IgE (type E immunoglobulins) upon first contact. The allergen sensitization phase is asymptomatic and the IgE produced binds to mast cells present in the dermis and in the gastrointestinal and bronchial mucous membranes. At each subsequent contact with the same antigen, the IgE transmit an activation signal to the cell, which triggers the allergic reaction by releasing inflammatory mediators such as histamine and arachidonic acid products (prostaglandins, leukotrienes, thromboxanes).
Histamine has a wide variety of pathological effects through the activation of its receptors, such as contraction of smooth muscle (e.g. reduction of the bronchial lumen), increase in vascular permeability (edema), increase in mucus secretion (runny nose and lacrimation), redness of the skin and itching.
The seasonal pollinosis are a typical example of a type I allergic reaction.
Me too'food allergy it is a type I allergic reaction, and has an incidence around 2% in the adult population. In children, the figure rises to 3-7%, although, in most cases, the allergy is overcome with school age. The foods that most commonly cause food allergy are: milk and derivatives, peanuts, fruit, shellfish, eggs, soy. When the allergenic substance comes into contact with the gastrointestinal tract, mast cells in the mucosa release histamine, which causes cramps, abdominal pain, vomiting and diarrhea.
In the severe condition of anaphylactic shock the presence of the allergen in the blood causes generalized activation of mast cells attached to the connective tissue of blood vessels; this causes a massive release of histamine and inflammatory mediators into the blood, causing increased vascular permeability and generalized smooth muscle contraction.
- Type II hypersensitivity reaction: these allergic reactions are mediated by free IgM and IgG antibodies, which no longer recognize the body's cells as their own, and develop aggression towards them, causing their destruction and causing an inflammatory reaction.
This can occur as a result of blood transfusions between incompatible blood groups (eg transfusion of AB positive blood in a patient with blood type 0 negative), or in maternal-fetal incompatibility (Rh). The administration of drugs that alter cell membranes also cause type II hypersensitivity reactions; penicillin, for example, binds to the surface of red blood cells, forming new antigenic determinants, recognized as foreign by the immune system. The consequence is the development of a reaction that causes hemolysis of red blood cells (breakdown of the red blood cell with the release of hemoglobin into the blood).
Autoimmune thyroiditis (Hshimoto's disease) is also a type II hypersensitivity reaction, produced by the action of specific IgG antibodies against the cellular components of thyroid cells (against the TSH receptor or thyroglubulin for example). A cytotoxic reaction mediated by T lymphocytes can also occur in Hshimoto's disease, causing destruction of the gland.
- Type III hypersensitivity reactions: they are diseases caused by immune complexes; immune complexes are formed between soluble antigens and IgG antibodies, present in the bloodstream. The deposition of these immune complexes in various parts of the body can cause an inflammatory reaction that is harmful to the surrounding tissues, as in the case of arthritis (deposition of immune complexes in the joints). Lupus erythematosus is also a chronic inflammatory disease caused by the deposition of immune complexes in connective tissues.
- Type IV hypersensitivity reactions: also called delayed hypersensitivity. Type I diabetes, rheumatoid arthritis, and multiple sclerosis are examples of autoimmune diseases caused by a type IV hypersensitivity reaction.
In contact dermatitis, T lymphocytes are activated in response to environmental substances that come into contact with the skin, such as nickel, cobalt and chromium. The first exposure to these substances does not generate symptoms, but causes the development of memory cells that will recognize the substance as a pathogen and will subsequently activate the immune response.
T-cell-mediated immune reactions provide extensive protection against bacteria, fungi, or protozoa, but can itself cause disease when T cell sensitization occurs by environmental chemicals or body cells. T-type memory cellsh1, once they come into contact with the allergen antigen, they are then able to recognize it, following subsequent exposures, and activate specific T lymphocytes (CD4 + and CD8 +), white blood cells capable of leading to death the cell target.

