Funzione e diffusione del colesterolo nell’organismo, il principale fattore di rischio per lo sviluppo di aterosclerosi ed altri problemi nell’uomo adulto.
Il colesterolo, una molecola di natura steroidea presente nel nostro organismo (Fig.1), è il lipide più conosciuto, a causa della correlazione tra livelli elevati nel sangue e le malattie cardiovascolari. Meno nota, anche se preminente, è invece la sua fondamentale funzione come component of cell membranes, how precursor of all steroid hormones, of the vitamin D and of bile acids.
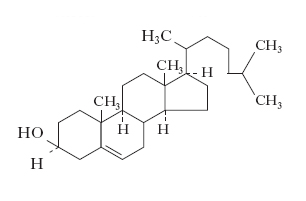
Fig. 1 - Cholesterol molecule
The most of cholesterol it is produced by the liver cells (hepatocytes), le quali sono in grado di produrlo autonomamente a partire da semplici precursori sebbene anche tutte le cellule dell’organismo siano in grado di farlo. Una piccola quota viene immagazzinata all’interno dell’epatocita, mentre la rimanente viene utilizzata o per la produzione degli acidi biliari oppure immessa nel circolo sanguigno per il suo utilizzo a scopo energetico da altre cellule del corpo, come ad esempio le cellule dei muscoli (myocytes).
Tutti i tessuti degli animali durante la crescita hanno bisogno del cholesterol per la sintesi delle membrane cellulari, mentre le ghiandole sessuali femminili e maschili (le gonads) lo utilizzano per produrre gli ormoni sessuali.
How is cholesterol transported in the blood?
All fats, the cholesterol and of triglycerides, due to their chemical nature they are not soluble in blood serum, which is instead aqueous, so to reach the tissues where its presence is required they must be conveyed into the blood plasma by transport proteins with which molecular complexes are formed, the plasma lipoproteins, consisting of a protein part (apolipoprotein) and another part of a lipid nature such as cholesterol and triglycerides.
Lipoproteins are classified according to density (g / ml) which varies according to the composition and the protein and lipid ratio:
- Chylomicrons, density <1.006
- VLDL (Very Low Density Lipoprotein), density between 0.95 and 1.006
- LDL (Low Density Lipoprotein), density between 1.006 and 1.063
- HDL (High Density Lipoprotein), density between 1.063 and 1.210
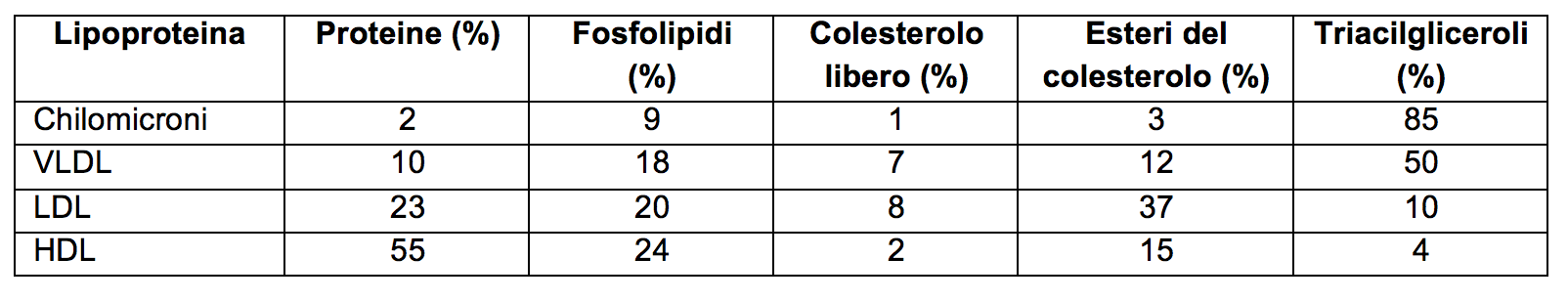
Tab. 1 - Composition (% mass) of the main human plasma lipoproteins
THE Chylomicrons they are deputies to the transport from the intestine to the tissues of fatty acids ingested with food, where they will subsequently be used to produce immediate energy or to be deposited as a reserve fuel. Once the fatty acids have been deposited, the chylomicrons return to the liver where they are degraded.
However, when we introduce more fats than necessary, the liver cells bind them to particular transporter proteins, forming the VLDL is LDL.
VLDL and LDL are released into the blood and have the purpose of reaching and depositing fatty acids in the adipose tissue, in the form of an energy reserve.
The LDL, being essentially the transporters of cholesterol, they are known by the term "bad cholesterol" as their concentration is sought as an index of risk of developing cardiovascular diseases, such asatherosclerosis.
Finally we find the HDL, produced by the liver and small intestine, which are high-density lipoproteins, consisting mostly of protein material, denser than lipids. They play a very important role in the prevention of cardiovascular diseases because they sequester and transport cholesterol to the liver where it will be transformed into bile acids, essential for the digestion of fats.
[More info] Biochemistry: endogenous biosynthesis of cholesterol
From a chemical point of view, cholesterol is an aliphatic polycyclic alcohol, and its brute formula is: C27H.45OH. All carbon atoms derive from a single precursor: theacetate.
Its structure with 27 carbon atoms implies a complex synthesis route, consisting of numerous biochemical reactions, which can be summarized in 4 main steps (Fig. 2):
1 Condensation of three acetate units to form the mevalonate, a six-carbon intermediate;
2 Conversion of mevalonate into isoprene units activated;
3 Polymerization of six isoprene units with five carbon atoms to form a linear compound with 30 carbon atoms: the squalene;
4 Cycling of squalene to form the 4-ring nucleus of steroids from which, through other biochemical reactions, the lanosterol, then finally the cholesterol at 27 carbon atoms.
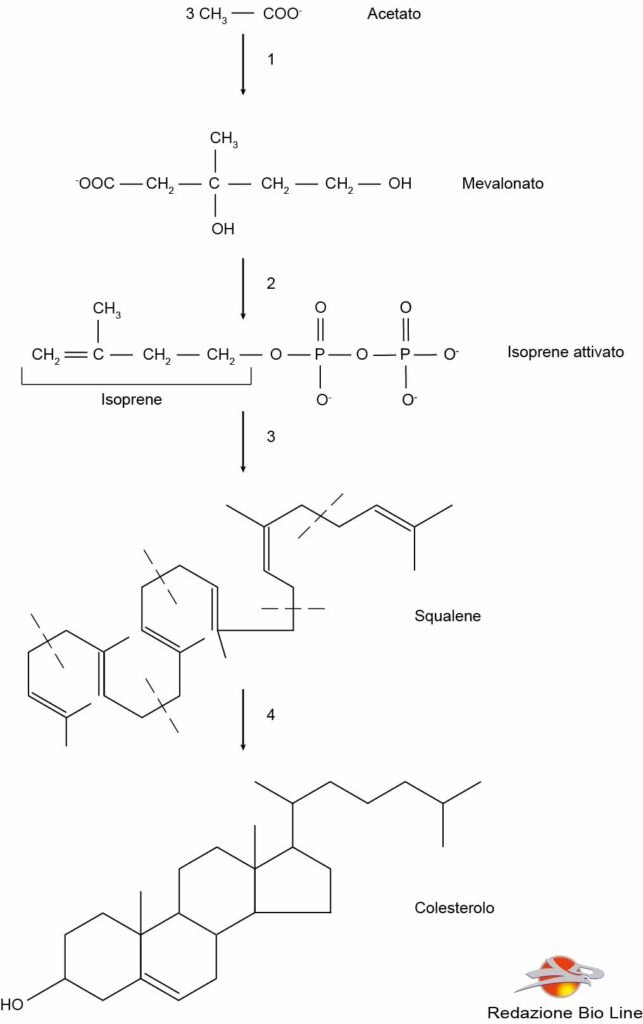
Fig. 2 - Biosynthesis of cholesterol
Atherosclerosis
L'atherosclerosis it is the first responsible for two of the three main causes of death in industrialized countries: myocardial infarction and cerebral infarction (stroke), the cause of which may be the uncontrolled production of cholesterol in the body. When the sum of cholesterol synthesized and that obtained from the diet exceeds the amount necessary for the synthesis of membranes, bile salts and hormones, the pathological accumulation of cholesterol in the blood vessels can lead to the formation of atherosclerotic plaques that can clog the arteries.
The atherosclerotic process is very complex and can be considered as a specialized chronic form of inflammation.
What triggers atherosclerosis is one endothelial dysfunction that is, a dysfunction of the internal tissue that covers the lumen of the vessel. The factors that cause endothelial dysfunction are:
1) lipid products (excessive cholesterol production);
2) combustion compounds found in cigarette smoke;
3) oxidative stress;
4) prodotti dell’infiammazione.
In response to these factors, the endothelium cells release: adhesion molecules, pro-aggregating molecules, cytokines, inflammatory mediators, etc ...
Alcune proteine di adesione richiamano monociti e linfociti che penetrano nella placca. Il colesterolo trasportato dalle LDL si accumula nelle zone in cui avviene il danno endoteliale, e, sequestrato dall’azione antiossidante degli elementi circolanti nel sangue, si ossida. L’ossidazione dei lipidi crea un’infiammazione nel sito di deposito, richiamando macrofagi e provocando il rilascio dei mediatori dell’infiammazione.
Il persistere dell’infiammazione genera la formazione di una capsula fibrosa che circonderà i macrofagi ed i lipidi fagocitati, isolando l’area danneggiata dell’endotelio; le cellule muscolari migrano nella tonaca intima dell’arteria, verso il lume del vaso: si moltiplicano e rilasciano collagene, elastina e matrice extracellulare, contribuendo ad accrescere la placca fibrosa, mentre i lipidi ossidati e le cellule morte saranno confinate al centro della placca fibrosa. La placca può continuare a crescere fino a provocare l’occlusione del vaso. Alcune condizioni come esercizio fisico pesante, un forte stress emotivo o malattie possono destabilizzare la placca, provocandone la rottura o il distacco.
Atherosclerotic lesions develop in order of frequency: in the abdominal aorta, in the coronary arteries, in the arteries of the leg, in the descending tract of the thoracic aorta, in the internal carotid artery and in the circle of Willis. Within each district there are also preferential locations of the plates, which can be explained according to the haemodynamic conditions of the blood flow: they are formed especially in the areas where the flow is not laminar, but whirling.

