Several birth control methods are put in place for prevent pregnancy. Some birth control methods work on a hormonal level by blocking ovulation (birth control pills), while others prevent the implantation of the zygote on the uterine wall (morning-after pill), still others, with a particular ethical impact, foresee the termination of pregnancy (abortion), causing the detachment of the cellular complex that will give rise to new life from the uterus.
Introduction: fertilization
In order for egg cell fertilization to occur, spermatozoa must be introduced into the female reproductive tract, no earlier than five days before ovulation, because that is the maximum survival time of spermatozoa, and the egg cell remains viable only 12-24 hours after its release from the ovaries.
The spermatozoa are unable to fertilize the female egg cell immediately, they will be after transforming, with the process called capacitation, inside the vaginal canal, in order to acquire the ability to fuse their outer membrane with that of the egg cell. This transformation process also allows the spermatozoa to accelerate the movement of the tail and to move more rapidly through the cervical canal towards the uterus; finally they enter the uterine tubes, attracted by the chemicals released by the egg cell.
Considering the ephemeral size of the spermatozoon (60 - 70 µm), a path even a few centimeters long inside the cavities of the female sexual organs actually represents an enormous journey, even 100,000 times its size, and the energy expenditure is so great. and the inhospitable acid environment (that of the vagina to ward off bacterial infections) in which they are found, causing the death of most of them. Of the millions of spermatozoa that are deposited, only a hundred normally reach the fallopian tubes while the others die along the way.
The surviving spermatozoa that will reach the egg cell inside the tubes will compete with each other and only one will reach the final goal, penetrating the barrier of the egg cell, fertilizing it (Fig. 1).
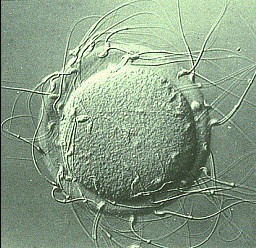
Fig. 1 - Sperm that surround an egg cell to fertilize it
After the fusion of the two progenitor cells, the cell membrane of the sperm disintegrates, and its chromosomes migrate towards the center of the cell. At this point, both the egg and sperm chromosomes combine, and the DNA is then replicated in preparation for the first mitotic division of the fertilized cell, now called zygote.
The fertilized egg undergoes many cell divisions and moves to the upper part of the uterus, where it adheres and penetrates the uterine wall, a defined event plant (Fig.2).
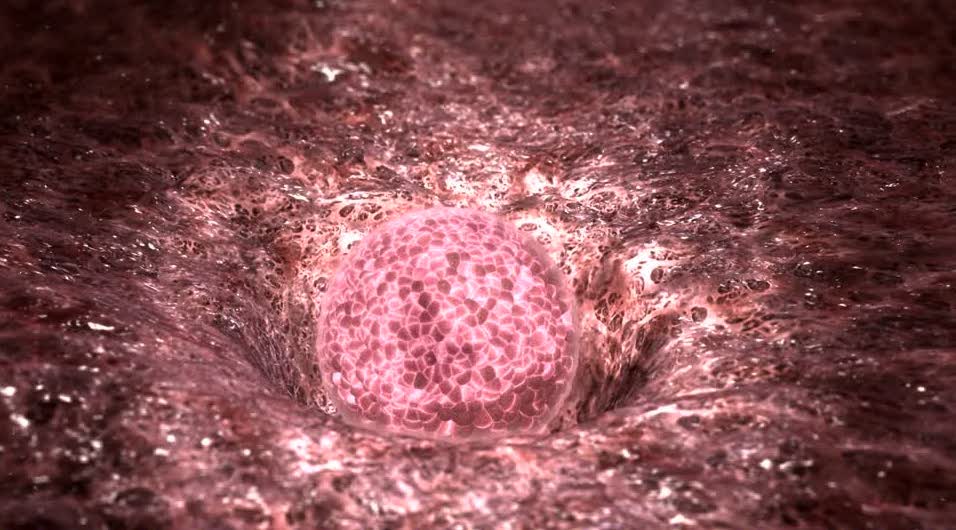
Fig. 2 - Uterine implantation of a fertilized egg cell
Contraceptive systems
Contraception refers to a series of methods or devices used to prevent conception. Some of the main birth control methods are listed below:
- Barrier systems: these systems are based on the use of special devices that act as a physical barrier to prevent the spermatozoa from meeting the egg cell. One such method is to place a thin rubber or latex sheath called condom on the man's penis. Another is to insert a diaphragm or capsule of rubber in the woman's vagina to be affixed before sexual intercourse.
The condom is the cheapest and most used contraception device, however it is not effective at 100%. It can prevent sexually transmitted diseases such as AIDS, however it must be considered that the HIV virus is very small in size, and there is a remote possibility (<99% of cases) that it can cross the latex of the condom.
- Contraceptive drugs: the contraceptive pill (or contraceptive pill) is a hormonal drug to be taken daily at the same time, and is the most effective reversible method of contraception.
- Uterine spiral or IUD: it is an intrauterine device, a small piece of metal or plastic in the shape of a T or Y that is inserted into the uterine cavity. Some IUDs contain copper or progestin drugs that are slowly released into the surrounding uterine environment. The copper released in loco kills any spermatozoa released into the vaginal canal during sexual intercourse. Furthermore, the presence of the foreign body in contact with the uterine walls causes a slight inflammation of the tissue that prevents implantation of the fertilized egg. The IUD can be effective for up to ten years and has less than 1% of failure.
- Spermicides: substances applied topically (gels, creams or vaginal pessaries), capable of altering the biological membranes of spermatozoa and causing their death. Spermicides can also be used as lubricants to be associated with barrier systems (eg condoms). The spermicidal substance most used for the formulation of these devices is Nonoxynol-9, a surfactant that degrades the lipophilic structure of the sperm cell membrane, dissolving it. Used alone, the spermicide is not considered a safe method of contraception, it is advisable to combine it with other methods such as condoms or birth control pills.
- Control of the basal rhythm: it is a very risky method and consists in predicting ovulation. It was a popular method in the 1970s but predictions are often based on a calendar, a daily measurement of a woman's body temperature (the temperature rises by 1 ° C after ovulation) and other signs such as changes in vaginal secretions. These methods, with the exception of the complete abstinencehave a relatively high failure rate; approximately 20% of couples experience unexpected pregnancy within a year.
- Coitus interrupted from the Latin coitus interruptis: it is a contraceptive practice that consists in the extraction of the penis from the vagina before ejaculation, in an attempt to prevent sperm from being introduced into the vagina. It is a natural contraceptive practice, but ineffective and can cause unexpected pregnancies. This is because prior to ejaculation, a small amount of lubricating fluid can come out of the penis during penetration and contain sperm that could fertilize the egg.
- Tubal ligation: a very effective contraceptive method which consists in placing clamps or rings to block the passage of the egg inside the uterine tubes (fallopian tubes), and prevent it from meeting with the spermatozoa. Unfortunately it causes in women the onset of an early menopause and tubal ligation can often cause a symptomatology known as "post tubal ligation syndrome", in which menstrual periods are longer and heavier than normal, cramps, back pain and extreme mood swings. However, the effectiveness of this method is close to 100% and the initial cost of the operation is amortized over the long term compared to the recurring cost of other contraceptive methods (purchase of birth control pills or barrier systems such as condoms and diaphragms).
- Vasectomy: disruption of the vas deferens that carries sperm from the testes to the urethra through their reversible ligation or through irreversible vasectomy leading to permanent sterility. This surgical sterilization system does not alter the erective capacity of the penis and still allows for orgasm and ejaculation to be achieved. However, there are possibilities to intervene with microsurgery and perform an anastomosis operation, or rejoining the dissected spermatic ducts, with the aim of restoring the fertility lost with vasectomy. However, only the 30% of interventions to restore the integrity of the spermatic ducts resulted in a pregnancy.
If the intervention to rejoin the spermatic ducts has not allowed to restore fertility, it is possible to use techniques for taking spermatozoa from the testicles or epididymis for intrauterine artificial insemination.
Permanent birth control methods such as vasectomy or surgical cutting or cauterization of the fallopian tubes are rarely used as conventional birth control systems are just as effective and less invasive. However, permanent sterilization may be necessary if a pregnancy could compromise the health of the mother, or if you do not want to transmit a hereditary disease or disability to the offspring. Finally, as already mentioned, generally the initial economic cost of a sterilization surgery is amortized over time, saving on the cost of contraceptive devices.
Emergency post-coital contraception techniques
There are emergency contraceptive methods to be implemented following a risky sexual intercourse. These systems consist in the intake of hormonal drugs, which can be administered in the hours (or days) after coitus, or after the deposition of the spermatozoa inside the cavities of the female sexual organs.
These drugs are not without side effects and must be taken under strict medical supervision.
- Morning-after pill
The best known medical specialty is Norlevo®. The drug consists of a single tablet (single dose) containing 1.5 mg of levonorgestrel, a progestin hormone. Levonorgestrel is a very powerful drug, so 1.5 mg represents a quantity of medicine that causes the ovulation process to slow down to almost stop.
The tablet should be taken as soon as possible, preferably within 12 hours, after unprotected intercourse and no later than 72 hours (3 days) after intercourse.
Norlevo® can be taken at any time during the menstrual cycle.
In the event that the egg cell was already fertilized and implanted, the drug would have no effect.
The following undesirable effects have been observed following administration of Norlevo®:
Very common side effects (affecting more than 1 user in 10):
dizziness, headache, nausea, abdominal pain, breast tenderness, menstruation delay, heavy menstruation, uterine bleeding, uterine pain, fatigue.
Common side effects (affecting 1 to 10 users in 100):
diarrhea, vomiting, painful menstruation.
Undesirable effects of unknown frequency:
cases of thromboembolic events (blood clotting) have been reported during the postmarketing period; allergic reactions such as swelling of the throat and face and skin rashes may occur after taking this medicine.
Currently in Italy Norlevo® requires a non-repeatable medical prescription only for underage girls, to be presented at the pharmacy, while it is no longer necessary to present the prescription for adult women.
- Five days later pill
The medical specialty is EllaOne®. The drug consists of one tablet (single dose) containing 30 mg of ulipristal acetate, which works by modifying the activity of the natural hormone progesterone, which is necessary for ovulation to occur. Consequently, EllaOne® works by delaying ovulation.
EllaOne® must be taken as soon as possible after sexual intercourse, and in any case within a maximum of 5 days (120 hours). Sperm can survive up to 5 days inside the body after intercourse.
Emergency contraception is not effective in all cases. Out of 100 women taking this drug, pregnancy occurs in about 2 cases.
Very common side effects (affecting more than 1 user in 10):
nausea, abdominal pain (stomach pain) or discomfort, vomiting, painful menstruation, pelvic pain, breast pain, headache, dizziness, body aches, back pain, tiredness.
Common side effects (affecting 1 to 10 users in 100):
diarrhea, heartburn, flatulence, dry mouth, unusual or irregular vaginal bleeding, heavy / prolonged periods, premenstrual syndrome, vaginal irritation or discharge, decreased or increased libido, hot flashes, changes in appetite, emotional disturbances, anxiety, agitation, difficulty falling asleep, drowsiness, migraine, visual disturbances, flu, acne, skin lesions, itching, fever, chills, malaise.
Rare side effects (which may affect up to 1 in 1,000 people)
genital pain or itching, pain during intercourse, ruptured ovarian cyst, unusually poor menstruation, loss of concentration, dizziness, tremor, disorientation, fainting, abnormal eye sensation, red eye, sensitivity to light, dry throat, taste disturbance , hives (itchy rash), feeling thirsty.
- Abortion pill
The active ingredient behind this drug is mifepristone. The drug was also known by the name RU-486 (from the manufacturer Roussel Uclaf); currently the medical specialty, which has the name Mifegyne®, is distributed in almost all Member States of the European Union (with the exception of Poland, Lithuania, Ireland and Malta), in Great Britain and in the USA.
Mifepristone is an anti-hormone that works by blocking the effects of progesterone, a hormone necessary for pregnancy to continue.
Mifegyne® is indicated for the following uses:
1) For the medical termination of an ongoing intrauterine pregnancy: no later than the 63rd day following the first day of the last menstrual cycle, in combination with a second drug, a prostaglandin (a substance that activates the contraction of the uterus and softens the cervix) to be taken 36-48 hours after taking Mifegyne®.
2) To soften and dilate the cervix before surgical termination of pregnancy during the first trimester.
3) As a pre-treatment before the administration of prostaglandins for the therapeutic termination of pregnancy beyond the third month of gestation.
4) To induce labor in cases where the fetus has died inside the uterus and in cases where it is not possible to use other medical treatments (prostaglandin or oxytocin).
Mifegyne® can cause the following side effects:
Very common (may affect more than 1 in 10 people):
contractions or cramps of the uterus, diarrhea, nausea or vomiting.
Common (may affect up to 1 in 10 people):
heavy bleeding mild or moderate gastrointestinal cramps, infection of the uterus (endometritis and pelvic inflammatory disease).
Uncommon (may affect up to 1 in 100 people):
lowering of blood pressure.
Rare (may affect up to 1 in 1000 people):
fever, headache, general malaise or tired feeling, vagal symptoms (flushing, dizziness, chills), hives and skin reactions which can be severe, uterus rupture following prostaglandin administration within the second and third trimesters of pregnancy, particularly in multiparous women (who have given birth more than once) or in women who have already undergone a caesarean section
Mifegyne® can also cause the following serious side effects: allergic reaction, rash, localized swelling of the face and / or larynx also accompanied by hives, severe or fatal toxic or septic shock, fever with muscle pain, tachycardia, dizziness, diarrhea, vomiting or feeling weak.
In depth: Mifegyne pregnancy termination procedure®
1- Swallow 600 mg (3 tablets of 200 mg) with a glass of water in the presence of a doctor or a member of the medical staff; Mifegyne® will be delivered to the prescribing center. If vomiting occurs within 45 minutes after taking Mifegyne® tablets, seek immediate medical attention. You will need to take the tablets again
2- Take the prostaglandin analogue, 36-48 hours after Mifegyne®. You will need to rest for at least 3 hours after taking the prostaglandin analog.
3- The embryo can be expelled within a few hours after taking the prostaglandin analogue or in the days immediately following. After taking Mifegyne®, vaginal bleeding will occur for an average duration of 12 days and the flow will gradually decrease in intensity
It is necessary to undergo a check-up within 14 - 21 days of taking Mifegyne® to check the health conditions and that the pregnancy has been completely expelled.

